Solutions for Medical Staff Professionals and Credentialing Teams
Expedite credentialing, privileging, and enrollment without adding staff
Access automated technology and expert CVO services to streamline credentialing processes and lighten your load.
Previously, I would have needed an additional three FTEs to achieve what my existing team can do with symplr Provider. Ask me any question about our providers and with a couple of clicks, I can give you what you need to know.
MEDICAL AFFAIRS DIRECTOR
Southern U.S. healthcare organization
Tackle your toughest medical staff credentialing challenges with symplr
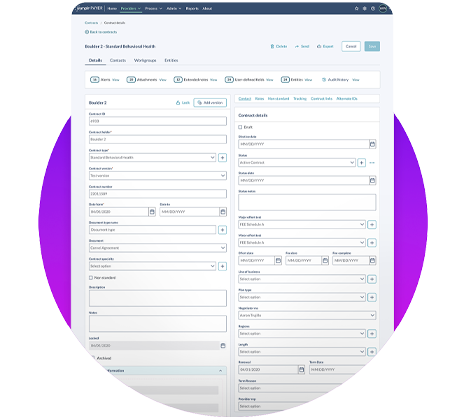
Rely on one source of truth for provider data
Say goodbye to data silos by collecting, verifying, storing, and sharing provider data in a single hub.
Credential providers up to 75% faster
Credential providers faster through automated primary source verification so members get access to high quality care.
Take the stress off staff and ease backlogs
Overcome staffing challenges by shifting primary source verification and payer enrollment to a trusted partner.
Deploy software that automates tedious tasks
Save time with an integrated platform that automates data entry and manages the entire physician privileging process electronically.
Spend 50% less time in committee meetings
Instantly generate a provider summary profile report and share it electronically to committee members to expedite the review process.
One partner to meet all your credentialing needs
The only end-to-end provider data management solution with 500+ credentialing experts to support you.

Experience the value of proven software with expert CVO services
Healthcare organizations who can credential providers to the best business standard reduce risk and protect patient safety.
However, antiquated processes and legacy software get in the way of successful credentialing and privileging. The result is slow onboarding, frustrated providers, delays in revenue, and overwhelmed staff.
Forward-thinking leaders are turning to modern, automated technology that accelerates workflows and Credentials Verification Organization (CVO) experts that lighten the load on understaffed credentialing teams.
Learn how symplr enables you to credential 75% faster and reduce credentialing time from the typical 90-120 days to 30 days.
Expedite credentialing and protect your health plan members with software created for payer organizations
Overcome challenges with siloed data, disparate systems, and poor data integrity.
Benefit from our highly configurable, end-to-end provider data management solution that leading payer organizations rely on for their single source of truth.
Gain peace of mind your data is protected with the highest level of security – HITRUST CSF certification. symplr Payer is the only provider data management SaaS solution to achieve this level of security.

Accelerate your credentialing with customizable services
Imagine if your team could reduce time spent on primary source verification, payer enrollment, and state licensure applications … and, instead, focus on clinical decision-making aspects of the privileging, peer review, and reappointment process?
Benefit from a partnership with symplr, the number one CVO in the industry. We custom-tailor services to meet your needs. With over 500 credentialing veterans, symplr CVO is the only team that is both accredited and certified by NCQA.
Our CVO team is your one source for primary source verification, payer enrollment, licensure, ongoing monitoring, and consulting, processing more than 7 million applications per year with zero failed applications.
Rely on experts from symplr to credential faster—and with confidence.

Drive efficiencies and reduce risk with automation in privileging software
Take your provider privileging process to a new level. Save time and reduce risk with automated, end-to-end electronic privileging. Integrate credentialing and privileging with quality (peer review, FPPE, OPPE) so you can monitor, benchmark, and report on provider performance.
Leverage an industry-leading privileging library containing more than 9,600 privileges across 320 specialties from over 40 trusted sources with embedded ICD/CPT codes to drive efficiency.
Track and manage requested privileges electronically.
Save time by consolidating privilege requests for multiple facilities in one form. Roll existing privileges forward and new privileges to be promoted.
Look who's achieving better outcomes with symplr
NILS LINDAHL
Provider Data Steward, Hennepin Health, Minneapolis MinnesotaEssentially, Complete Health's investment in symplr CVO paid for itself in weeks. We realized an ROI almost immediately and were able to use the savings for other initiatives.
JIM MIHNOVICH, CFO
Complete Health64% of medical staff services professionals reported that turnover is impacting workload, leading to insufficient staff resources


