Midas DataVision
Access risk-adjusted, enterprise-wide quality indicators and regulatory measures
Benchmark performance and quality with comparative, risk-adjusted data. Track and analyze clinical utilization and provider practice patterns. Evaluate high-risk populations. Meet legal and accreditation reporting requirements. Predict readmission penalties.
We can look at data across all our markets for our primary care population. We’re able to look at different data sources and do more advanced analytics, like [generate] composite clinical risk scores to stratify our populations.
Director of analytics and technology
Analytics built for healthcare to drive clinical and financial operational performance
Improve financial performance and reduce penalties
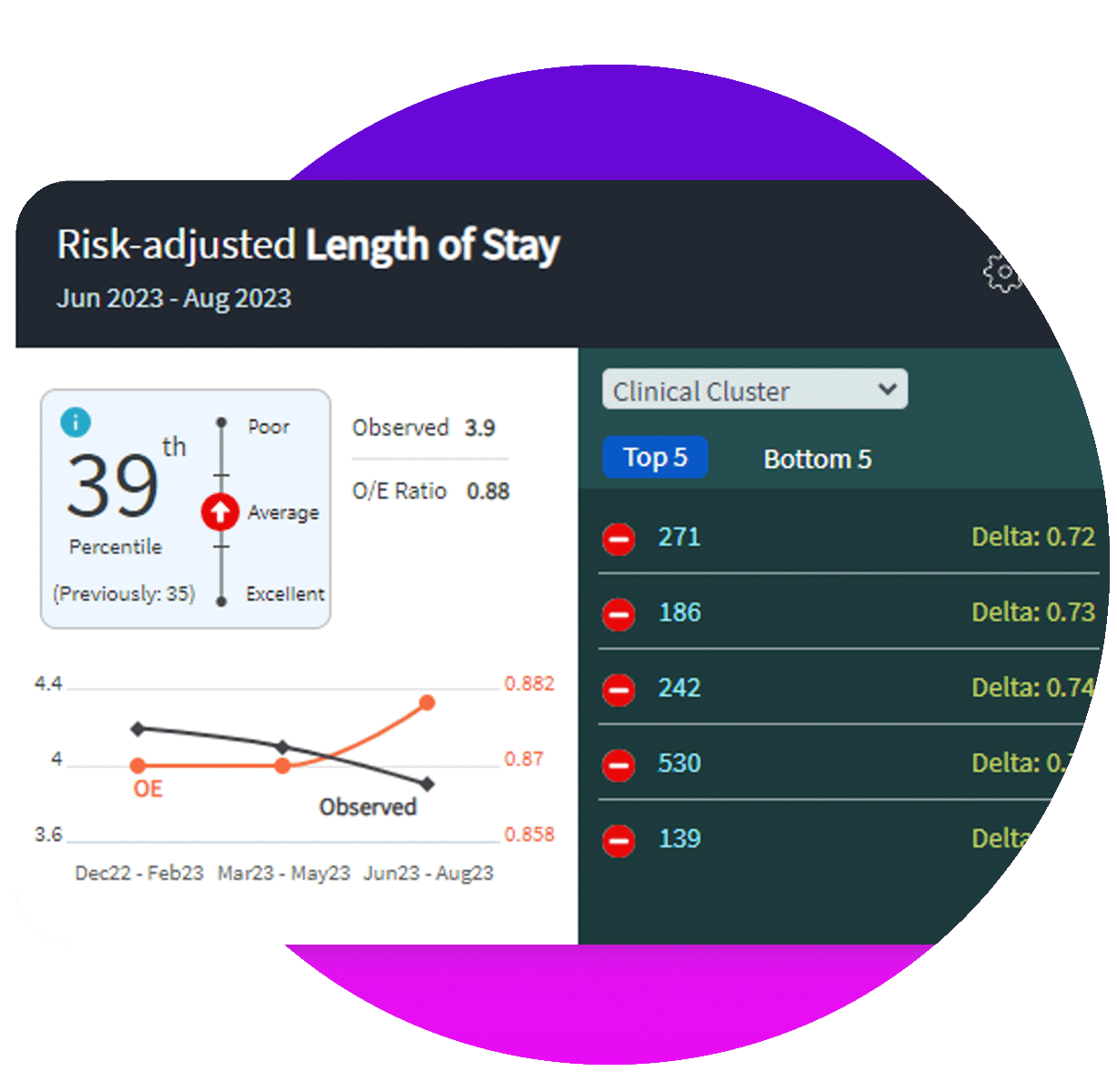
Cut costs by decreasing length of stay, unnecessary admissions, treatments, and readmissions. Increase visibility to reimbursements, potential penalties, write-offs, risk of litigation and claims losses by improving clinical processes adjusted for volume and severity.
Improve performance, quality, safety, and patient outcomes
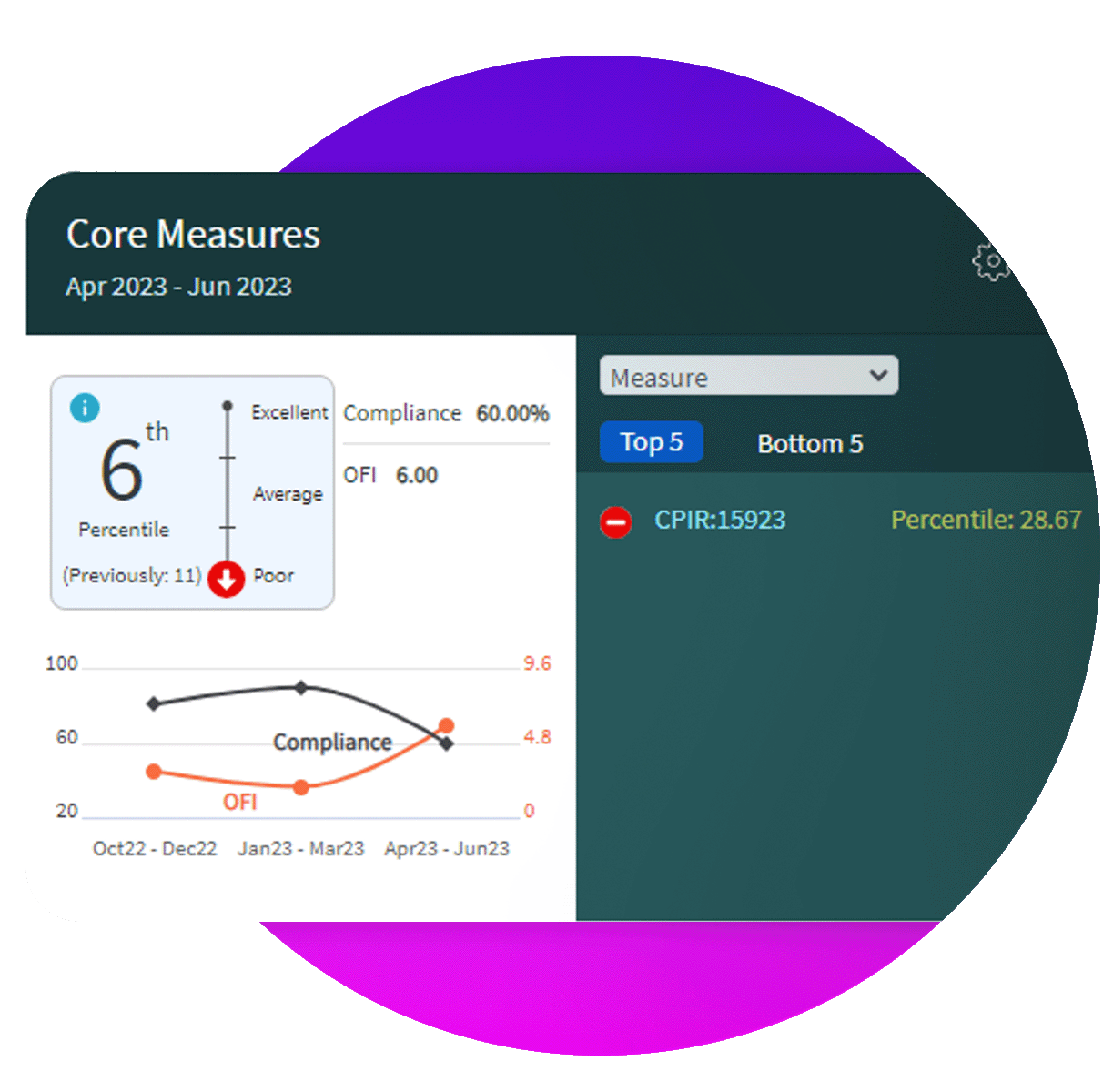
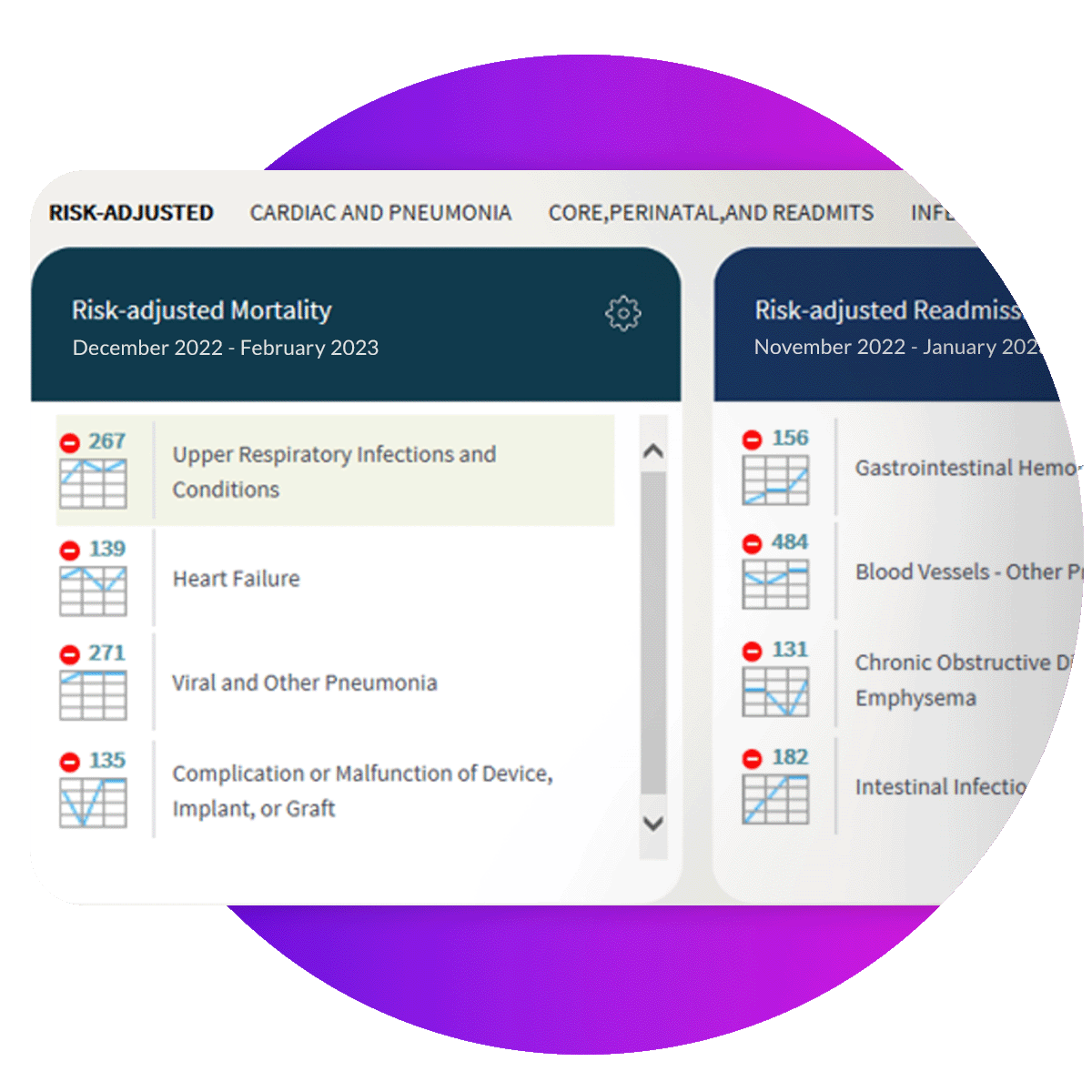
Uncover opportunities to improve, special cause signals, exemplary performance, complications of care by measuring clinical outcomes, processes of care, care management efficiency, resource utilization, coding compliance, and patient safety. Benchmark performance compared to peers with risk-adjusted quality indicators and one of the nation's largest comparative databases for hospital quality available.

Can you access current, risk-adjusted data across care settings to measure performance and quality?
More than ever, managing healthcare means managing data—to measure and improve patient outcomes and navigate regulatory requirements. Healthcare leaders and clinicians must make data-driven decisions when delivering patient care and need real-time, risk-adjusted data to drive decision making.
Driving quality improvement and change takes current, credible data that clinicians trust. When data is outdated and spread throughout multiple sources and systems, quality is difficult to measure and maintain. Lagging quality and risk data negatively affects critical decision-making, resulting in quality of care also suffering.
As quality outcomes are increasingly tied to reimbursements and financial penalties, access to current quality data and patient outcomes is still not enough. Clinicians need holistic, actionable analytics benchmarked against care standards to take fast and decisive action. Outdated quality and risk data prevents the best patient outcomes.
A true healthcare-specific analytics suite to help drive clinical and financial performance
Access the information you need to improve clinical outcomes and achieve hospital pay-for-performance targets
Track and analyze clinical utilization and provider practice patterns, evaluate high-risk populations, and meet legal and accreditation reporting requirements - as well as access disease-specific registries and surveys.
- Make critical decisions using risk-adjusted data down to the patient level that practitioners trust
- Harness the power of advanced machine learning algorithms including risk adjustment models, the Readmission Penalty Predictive Analytics for HRRP, Value Based Purchasing, and clinical treatment targeted profiles for quality and data improvement
- Identify opportunities for improvement, special cause signals, areas of exemplary performance, rare events, and complications of care
Benchmark against national standards and peer organizations
Midas DataVision enables you to benchmark against similar organizations for stronger comparisons, data accuracy, and common goals. Accelerate your decision-making by comparing severity-adjusted outcomes data from one of the nation’s largest concurrent databases and effectively share across your organization using standardized reports, indicators, and tool packs.
- Stratify practitioner and facility performance compared to peer hospitals and adjust for patient-centered risk
- Access more than 21,000 prebuilt metrics aligned with national quality reporting programs and provider-specific outcomes with drill downs to patient-level data
- Compare against peers for selected time periods (month, quarter, and calendar year) and for facility characteristics (such as bed size, case mix, region, and teaching status)
- Navigate and use data analysis functions for more than 50 clinical case types intuitively organized by clinical product line and disease
Make it easier to gather data and create reports for accreditation and regulatory requirements
Compile the data and generate reports you need for timely submission to accrediting bodies and regulatory agencies.
- A full suite of functions for the data collection and submission required for acute care inpatient, hospital outpatient, and behavioral health regulatory topics as defined by The Joint Commission and the Centers for Medicare & Medicaid Services (CMS)
- Integrate National Hospital Quality Measures with physician profiles and other custom profiles
- Track and trend performance for clinical process of care, outcome and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) patient satisfaction measures
- Identify cases with hospital-acquired conditions designated by CMS as potentially affecting MS DRG assignments and calculate potential financial impact
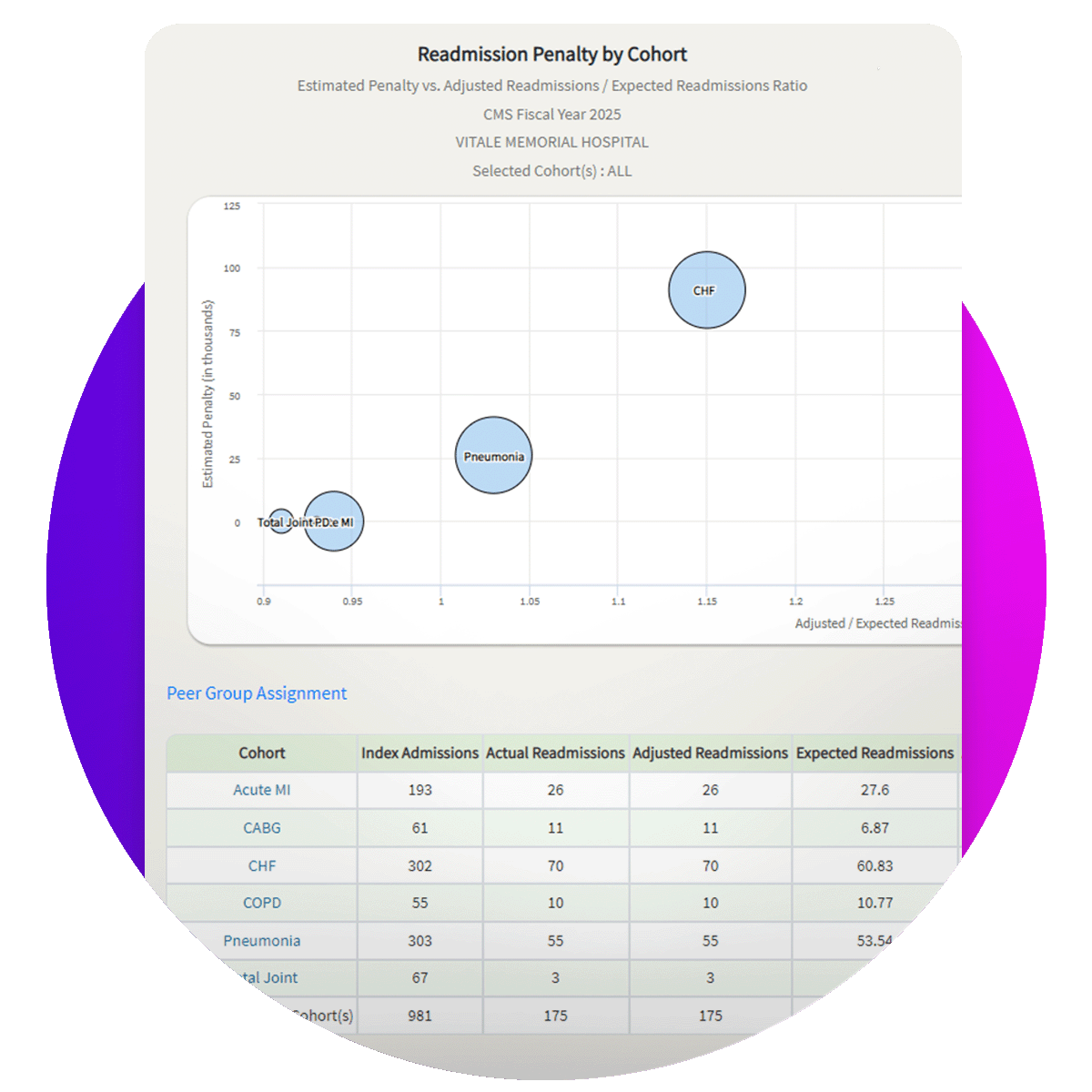
Anticipate excess hospital readmissions and potential penalties before the performance period has lapsed
DataVision’s Readmission Penalty Forecaster helps hospitals anticipate their excess readmissions and potential Hospital Readmissions Reduction Program (HRRP) penalties from CMS before the performance period has elapsed. Be proactive in your performance improvement and care transition strategies for the six populations being evaluated by HRRP.
Predictive Insights
Replicate CMS’s readmission risk models and penalty calculations up to three years before you receive your excess readmission reports from CMS
Identify Problem Cohorts and Trends
Prioritize your hospital readmission reduction strategies today for those clinical populations with the greatest risk for financial penalties tomorrow
Reduce Readmissions and Penalties
Use actionable advice to inform performance improvement strategies
Ready to learn more about Midas DataVision? Let’s chat.
Get in touch

Improve standards of care while reducing risk and financial penalties
A full suite of analytics to drive up healthcare operational performance
Midas Comparative Performance Measurement System
A full suite of functions for the data collection and submission required for acute care inpatient, hospital outpatient, and behavioral health regulatory topics as defined by The Joint Commission and CMS. Data submission services are available to support reporting to many state-specific initiatives.
DataVision Report Tool Pack
Export encounter-level detail for selected populations that includes resource utilization profiles with more than 260 data fields.
Midas Proprietary Risk Model
Identify more or less preventable risks related to LOS, mortality, readmissions, and complications for Clinical Clusters, including calculations of potential lives, days, readmissions, and complications saved.
DataVision Risk Management Tool Pack
Analyze the volume and location of risk events by event type class, risk event class or clinical population for patients and nonpatients.
Care Management Efficiency Analysis
Review the unique radar graph to compare performance against peer hospitals for readmission rates, admission rates, one-to-two-day LOS, charges and discharge to alternative levels of care.
Value Based Purchasing
Track and trend performance for clinical process of care, outcome and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) patient satisfaction measures.
CMS HAC Financial Impact
Financial Predictor Reports – Identify cases with hospital-acquired conditions designated by CMS as potentially affecting MS DRG assignments and calculate the potential financial impact.
Acute Care Comparative Scorecard
Uses selected criteria to award points to hospitals based on their performance and ranking among their peers.
Insights Dashboards
Increase operational efficiency, reduce costs, and improve quality performance with three insight dashboards – Readmission Insights, Sepsis Insights, and Executive Insights. Providing you with a quick snapshot of your organization’s data without having to run additional reports and complex data analysis.
Get With The Guidelines
Send Heart Failure core measure data, Stroke core measure data, and additional fields to IQVIA.
Ambulatory Measures
Easily track and analyze clinical utilization and provider practice patterns, evaluate high-risk populations, and monitor performance on key ambulatory metrics.
Midas DataVision Gateway
Allow Midas DataVision data to flow into corporate level dashboards and bring technology-driven insights into the forefront of the patient care environment.

-3.jpeg?width=2000&name=Blog%20Image%20Template%20(1)-3.jpeg)
