Social Determinants of Health Examples: Quality and Payments


The conditions in the environments where people are born, educated, work, play, and go about their lives greatly affect their access to healthcare, their health risk factors, and ultimately their health outcomes. You're likely hearing more about this not just because ensuring health equity is an important societal issue, but also because social determinants of health (SDoH) are being tied to quality healthcare and payments.
Defining social determinants of health
We know that the non-medical factors and conditions that surround a person or a population affect health equity and set the stage for unequal access to healthcare and potentially poorer health results. For example, racial differences in mortality rates persist despite initiatives to correct inequalities. However, the shift to value-based payment in healthcare links reimbursement to outcomes. As a result, payers and provider organizations are incentivized to act on data related to social determinants of health.
Population health, public health, health equity & social determinants of health: What's what?
|
The five domains of SDoH
Thousands of factors affect a person’s health. But to better study the contributing elements, the U.S. Department of Health & Human Services (HHS) and its major operating components (e.g., The Centers for Disease Control and Prevention, The Centers for Medicare & Medicaid, and The Office of Disease Prevention and Health Promotion) established five domains of social determinants of health: 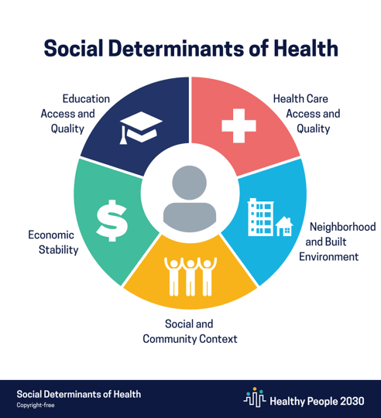
- Neighborhood and built environment
- Social and community context
- Education access and quality
- Economic stability
- Healthcare access and quality
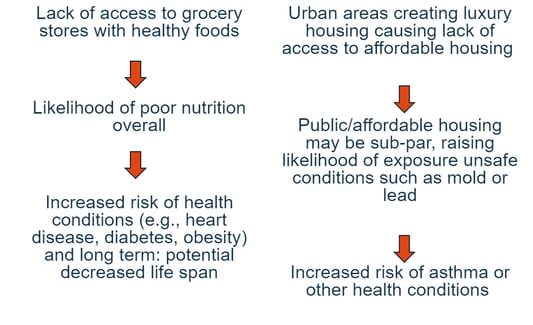
Delve into the domains and one can begin to see how negative circumstances affect people’s health. Examples include unsafe housing, lack of public transportation, racism or other discrimination, violence, lack of educational opportunity, income disparities, polluted air/water, language barriers, and illiteracy. And studies show that there’s a cascade effect of any one (or multiple) of these disparities. For example:
Patients’ view of social determinants of health
Patients don’t always think about their risk factors for health outcomes in the same terms as healthcare organizations and regulatory bodies do. To them, social determinants of health are represented in daily challenges, especially if their basic needs aren't met. An astounding 40% of people in the U.S. today don't have adequate access to:
- Nutritious food
- Clean, running water
- Heating/air at home
- Money for prescriptions
- Transportation
- Phone/computer
- Access to care (e.g., live in a rural area)
And many face challenges like these on top of lacking basic needs:
- Illiteracy (Can the individual read medical labels/instructions?)
- Socialization/loneliness (Does the person have family/caregivers?)
- Mental illness/depression (Is the individual being treated for these pervasive health issues)?
COVID-19, especially, focused attention on social determinants of health and heath equity. Many eyes were opened to the inequity of basic needs based on class, race, geography, and other factors.
A spotlight on quality
Improving the health of all citizens benefits everyone socially and economically. But a confluence of factors is giving the government and the private sector special incentive to address social determinants of health and reduce health disparities. The issues cross quality, safety, and reimbursement, and include:
- The cost of healthcare continues to rise sharply, despite many initiatives to stem costs
- Our healthcare delivery and payment systems are posting insufficient return on investment for government and some provider organizations, and there is room for price gouging
- Heightened awareness of social justice issues is leading more individuals and companies to act through demands or initiatives
- Healthcare reform requires payers and provider organizations to work more closely together. In managed care space, social determinants of health was always at the forefront
- There are many more opportunities today for entities beyond government and healthcare to get involved in social inequity
The changes we make today will affect quality and reimbursement for all healthcare organizations down the road.
Barriers to addressing social determinants of health
It’s no easy task to address the structural issues that result in unequal access to healthcare and poorer health results among some Americans. For example,
- Initiatives across education, housing, literacy, legal, etc. have not always connected to help those who face healthcare and other disadvantages.
- The data and technology needed to coordinate efforts are siloed in government and state agencies, healthcare organizations, commercial enterprises, and payer organizations such as MCOs.
- Programs that have been successful within communities have been difficult to replicate at a larger scale.
But there is progress among organizations whose goal it is to connect the dots, especially with regards to social determinants of health. For example, the Office of the National Coordinator for Health Information Technology, a part of the DHHS, is making strides. And there is slow but sure movement of corporations/CEOs who care about fiscal and social good (i.e., “do well and do good”) in their communities.
Simply put, today there is more opportunity for shared accountability regarding healthcare inequities—and the future of value-based payment demands it.
Technology—and a dichotomy
Today’s technology can be used to screen, identify, prioritize, connect, and support patients with social determinants of health needs, as well as identify and prevent risks. COVID-19 drove a 50–2,800 per month average increase in telehealth visits at healthcare organizations, and brought telemedicine to the forefront of healthcare.
Yet telemedicine also spotlights the work still to be done to address social determinants of health and inequities in healthcare. According to William Torkildsen, MD, Chair of the Valley Organized Physicians, a Texas-based independent physician association: “While virtual healthcare has gained a tremendous push recently, we’re finding telemedicine literacy is a challenge ... only 40% of our Medicare patients are 'virtually fluent’.”
Other challenges abound, again stressing the need that community resources must unite to address health equity issues and social determinants of health:
- Patients spend only one hour per year annually in exam rooms
- Patient data is not always updated online, and exists in too many disparate places
- Despite HIPAA regulations, technology leaks personal patient information, leading to harm or distrust
- There could be an adjustment to patient perception of “caring” as physicians deliver more services online only
The future of SDoH with payers
It’s clear that payers’ and providers’ attention on social determinants of health will only increase going forward. For example, Patrick Conway, MD, now CEO of Care Solutions, Optum at UnitedHealth Group, has historically invested in social determinants of health at the healthcare organizations he leads. And he’s not alone. Kaiser Permanente has been addressing social determinants of health for years, even building affordable housing; and Cerner CommunityWorks offers free telehealth access for rural hospitals.
Social determinants of health are not new, but they're now at the forefront of addressing healthcare inequities and will remain as a new normal in healthcare. Learn how symplr's solutions can help your provider or payer organization track and incorporate essential data today.
