Provider Data Management | symplr CVO
Fast, accurate credentialing and payer enrollment services

+7 million applications successfully processed each year
Our NCQA-accredited and certified credentials verification team has decades of experience. The result: zero failed applications.

Overcome your staffing challenges, onboard physicians faster, and speed up the revenue cycle
Under tight operating margins, staffing challenges, and inefficient credentialing and payer enrollment processes, many healthcare organizations are focused on delivering more work in less time.
The backlog of work has always existed, and while it might be growing, it's not something most organizations are capable of addressing with current resources.
But the backlog and inefficient processes have real downstream effects on the bottom line, operating margins, patient safety, and provider satisfaction.
symplr CVO provides flexibility to address your backlog and scale your credentialing and enrollment processing power. You can choose to delegate your entire provider credentialing and enrollment workstreams, or just a portion of them. Our experts work alongside you to support your team with complete, unmatched visibility into our processes.
Take the stress out of credentialing and expedite enrollment with confidence
Realize revenue faster
Get 100% transparency into provider statuses
Shorten the licensure application process
Cover all your credentialing needs with a proven partner
Primary source verification services
Payer enrollment services
Licensure services
Committee management support
Delegated credentialing agreements
Hospital privilege application process
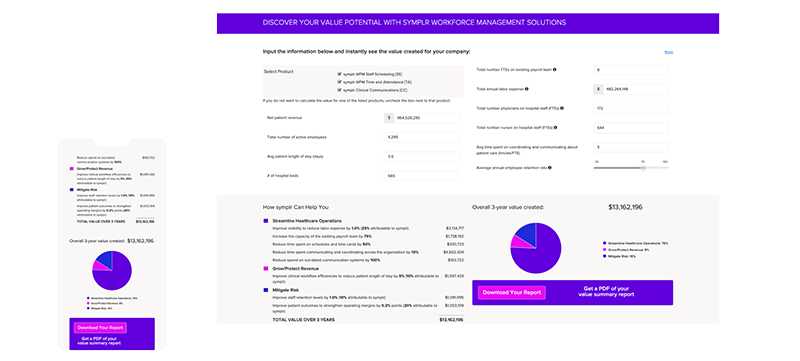
The numbers don’t lie: See the value symplr CVO would add to your organization
See what our customers are saying about symplr CVO Services
symplr CVO assisted with license requirements research and contributed to the improvement of our internal licensing process, remaining attentive, professional, and flexible in response to shifting priorities along the way.
symplr has successfully tackled our most complicated practice structures...the depth and breadth of their team has been instrumental in our growth and success. I highly recommend their services and partnership.


