Stabilize Your Health System with a Strong Workforce Management Strategy
With all of the chaos, uncertainty and change in the healthcare industry, you need your workforce management strategy to be a stabilizing force. By focusing on developing a workforce management strategy that impacts staff engagement, quality of care, and labor cost containment, you build organizational resilience.
A strong workforce management strategy provides the foundation health systems need to navigate the challenge of delivering quality patient care with shrinking budgets. Strategies that worked just a year ago need to be revamped in the face of a wildly different set of circumstances. To meet these new challenges, we’re seeing our customers looking for ways to capture more value from their staffing and workforce initiatives.
We recognize that health systems need more from their workforce management strategy. In response to our customer's needs, we’ve developed a process that helps health systems adapt their workforce management strategy to achieve balanced outcomes, contain costs, improve patient care, and engage staff, even as their circumstances and needs change. This framework is called the Ongoing Process Improvement Loop.
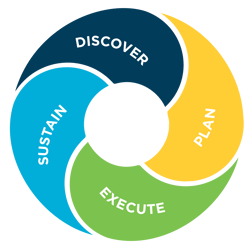
Here’s a closer look at each step of the Ongoing Process Improvement Loop that has delivered results for our customers.
Phase 1 - Discover
This process starts with the discovery of gaps between goals and outcomes. Together with your team, we look at desired goals compared to actual outcomes, digging into the areas where there are performance gaps. We go beyond just spotting the problems; we also pinpoint the root causes so we can understand why the performance gaps are happening. During this stage, it’s important to take a deep dive into the analytics and carefully examine the processes, policies, and governance structures that are impacting the data and the outcomes.
Here are just a few areas we examine during the Discover phase:
- Are your patients covered by the right number of staff with the right skill mix?
- Are you spending payroll dollars efficiently, with minimal premium pay?
- Do employees have predictable, flexible schedules?
- Are you using staff, patient, and unit data to effectively flex staff up and down before and during each shift?
- Are you fully leveraging your workforce management technology to help solve your organization’s business challenges?
Phase 2 – Plan
With an understanding of the performance gaps and the root causes for those gaps, we work together to develop a Plan to address the issues. The Plan accounts for each customer’s unique needs while also applying the leading practices our team has developed over the last 35 years of working with hospitals and health systems.
Here’s how one of our Customer Outcomes Executives, Dan Gorman, explains the importance of a comprehensive, up-to-date current plan:
“With the healthcare industry facing more demands than ever before, our clients need more from their workforce management solutions. Strategies that worked three or five years ago, or even just a year ago, need to be adjusted to manage a new set of problems.”
The Planning phase includes helping customers understand the full capabilities of their workforce management technology so they are in a better position to make decisions that improve staff satisfaction, the patient experience and the bottom line. Equally important is understanding how the technology can support their goals around process improvements, staff engagement, and enterprise-wide collaboration.
Phase 3 – Execute
During the Execute phase, the need to focus on technology set-up, staff training, implementation, and go-live is both logical and essential. Equally important is managing the impact these changes have on the staff. A workforce management strategy impacts every employee within the health system, and there are a lot of stakeholders. Therefore, a clear plan for change management should not be overlooked, but it often is.
According to Minhchau Scaljon, our Services Director,
“Leading people through accepting change is one of the most frequently neglected activities in healthcare IT projects. We want to be sure our customers are addressing the people aspect of change to get the most benefit possible from our solutions. That’s why we’ve developed a program that provides the knowledge, guidance, and tools to help our customers support their organization through change.”
Phase 4 – Sustain
As shown in the Ongoing Process Improvement Loop, successful initiatives do not end with execution and go-live. Instead, we continue to work with our customers to ensure continuing outcomes and stronger organizational resiliency.
The keys to the Sustain phase are shared governance and a culture of accountability. When all stakeholders have been engaged throughout the Discover, Plan, and Execute stages, the goals of the initiative and everyone’s role in achieving those goals have been defined and agreed upon. That clarity creates ongoing collaboration, shared accountability, and sustained success.
The CNO at a multi-state health system in the Midwest summed this up perfectly:
“The success of a workforce management initiative is 20% technology and 80% operational. If the solution isn’t working, the first thing we need to look at is whether or not it’s being implemented and used correctly. Ultimately, the project’s success depends on the culture and leadership.”
Success Story: Culture of Accountability Delivers Sustainable Outcomes
One of our customers, a 6000-employee health system in the South, needed to find a way to accommodate increasing volumes without adding more beds. They have resolved their throughput issues by building a culture of accountability that supports both sustained outcomes and strong employee engagement. By focusing on integrated workforce analytics, they’ve realized efficiency gains and strong financial outcomes – all while being recognized for their high levels of staff engagement.
Here’s a closer look at how the Ongoing Process Improvement Loop has delivered results:
DISCOVER: The data showed a 10% increase in inpatient volumes, and that discharges from inpatient units were slower than the health system wanted, with about 20% of discharges happening before 1:00pm. A deeper look at processes showed that admissions were happening before discharges left, causing bottlenecks in the emergency department.
The organization recognized a need to develop a capacity project that focused on people, process, and technology to somehow create more capacity without building more beds. The team also saw a need for managers to be more productive and manage their volumes more efficiently.
PLAN: The team developed a two-part plan to address the issues they had uncovered.
The first part of the plan was to create capacity with a logistics center, which centralized all patient placements and clinical logistics. The logistics center includes the roles of Patient Flow, Hospitality Flow, External Transport, Discharge Expediters, Admission Team, and LPN Resource Team.
The second part of the plan focused on an integrated workforce management strategy that would give managers the accurate, timely data they needed to make smart, proactive staffing decisions. This strategy started with providing staff with the technology tools they needed to be accountable for their own time and attendance data, including clockings and timecards. That staff accountability helps managers in two ways. First, managers spend less time updating and correcting employee data, allowing them to be more productive. Second, they have access to accurate, up-to-date time and attendance and staffing information so they can better manage their unit’s productivity.
EXECUTE: Because the success of the initiative depended on both staff and managers doing things differently, change management was a top priority. The team used the Kotter Change Model, which is focused on driving action by appealing to both the head and the heart. This approach was important because paychecks and schedules are extremely important to employees.
Other factors that were key to the initiative’s success:
- Recognizing that nursing managers are not accountants or analysts, so they needed to be provided the training and tools necessary to meet expectations.
- Developing Super Users and peer resources, so everyone could connect with relatable people whenever necessary.
- Creating strong relationships and open communication between nursing and finance.
- Gaining staff buy-in through organizational consistency.
- Ongoing support and buy-in from the Board and Financial Team.
- Helping managers and the entire organization achieve wins with a powerful analytics tool focused on productivity metrics.
This initiative delivered big wins for the organization both operationally and financially. Success metrics include:
- $8.8M in savings over three years through better staffing decisions and efficiencies realized from increased volumes.
- Decreasing patient placement time out of emergency department by two hours and increasing discharges before 1:00pm by 20%
- Creating a Departure Lounge used by 35,000 patients annually. That freed up 7,000 hours of bed time, the equivalent of a 30-bed unit.
SUSTAIN: By developing a culture of accountability, the health system was able to focus on correcting actions that were outside of established expectations. For example, managers are responsible for timely timecard approvals, and the CFO sends out an email to the managers that fall outside of the acceptable percentage of timecard approvals. For those who are continually non-compliant, the CFO speaks with them individually.
Staff are accountable for signing off on their timecard at the end of the pay period and clocking in and out at the beginning and end of each shift. If they forget, they must request a correction from their manager immediately. If the correction is not done by the close of payroll, the employee will not be paid for that shift until the next payroll.
This culture of accountability is a staff satisfier for the organization, with both managers and staff appreciating the standardization and consistency across the entire enterprise.
Check out more customer success stories here.
Learn more about our solutions and services here.