Real-Time Provider Data and Medical Staff Office Efficiency
Provider data powers healthcare in countless ways, making the successful management of it crucial for all healthcare participants. For starters:
- Patients rely on accurate, up-to-date directories to choose in-network providers who are conveniently located and provide specialized services.
- Providers submit their data to be credentialed and privileged to treat patients.
- Health plans and health systems need accurate provider data for referrals, claims payment, payer/provider contracting, network management, and provider performance monitoring to deliver or enable safe, high-quality care.
But challenges abound when it comes to efficiently maintaining accurate provider data. Physicians and other clinicians move to a different networks or add services at another site in the same system. They retire, leave or join health plans—or in some cases, lose their license. These statistics from an IDC Health report tell the story:
- About 2% of provider demographic data changes each month
- Some 20-30% of providers change affiliations each year
- Roughly 5% of physicians undergo a status change (e.g., retire, die, lose a license, or are sanctioned) annually
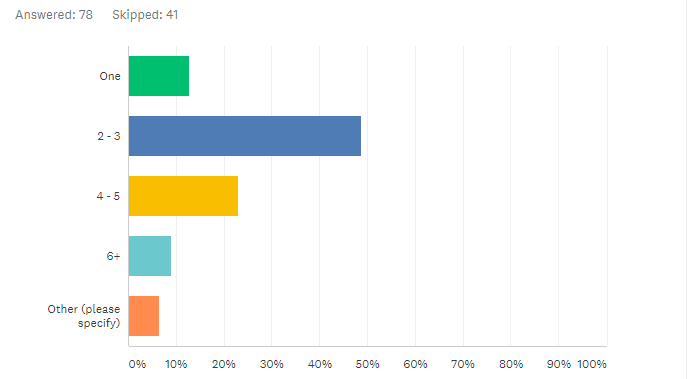
Given these changes, it’s no surprise that the provider data stored in the multiple software solutions that hospitals use to house it is incorrect. A survey of hospital medical staff offices by symplr in May 2021 found that roughly 58% of medical services professionals (MSPs) (55 of 77 people responding) reported using two to five solutions for their job, despite the fact that technology that integrates all provider data is available.
Q: How many solutions do you use to complete the provider data lifecycle including recruitment, onboarding, credentialing, privileging, enrollment, evaluation, and re-credentialing?
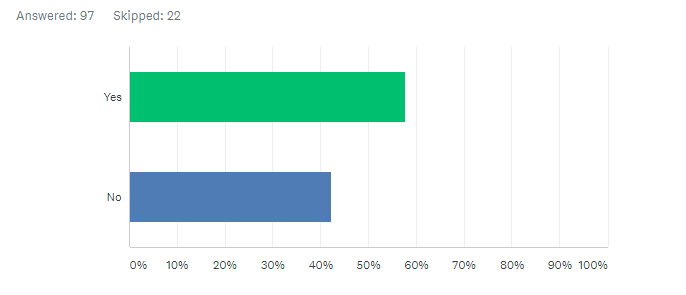
Further, 43% of MSPs (41 of 96) in symplr’s survey said they lack timely access to data they need.
Q: Does your medical staff office have real-time access to the data required for every phase of the provider lifecycle (e.g., onboarding, credentialing, privileging, enrollment, evaluations, etc.)?
Provider data accuracy isn’t much better from the patient perspective: According to an American Medical Association survey, more than half of U.S. physicians find that their patients encounter health insurance coverage issues at least once a month due to inaccurate directories of in-network providers. And a Centers for Medicare & Medicaid Services’ (CMS) review of 52 Medicare Advantage Organizations’ online provider directories (with a total of 5,602 providers reviewed at 10,504 locations) revealed that 49% of the directory locations listed had at least one inaccuracy. Typical inaccuracies included:
- The provider was not at the location listed
- The phone number was incorrect
- The provider was not accepting new patients when the directory indicated they were
In response to the review, CMS issued 18 notices of non-compliance, 15 warning letters, and seven warning letters with a request for a business plan.
The high cost of poorly managed provider data
Poor provider data management, resulting in inaccurate provider data, hinders patients’ access to care and is costly in consequential ways, including the following:
- Patient dissatisfaction: Patients may spend a significant amount of time finding a doctor in their network who meets their needs, only to discover that the provider moved to a different office a year ago. Frustrated by that experience, the patient may choose a physician in another healthcare organization. Meanwhile, your healthcare organization loses revenue from missed/canceled appointments (when the patient realizes the in-network physician is no longer at that location).
- Provider onboarding delays and resulting revenue loss: Incomplete or inaccurate information regarding a provider’s credentials—work, professional certifications, malpractice insurance, or other required details—can cause extensive and expensive delays. Medical staff personnel must track down the correct information or wait for the provider to supply it. Credentialing and enrollment delays are costly in terms of postponed reimbursements, reduced member access, and frustrated providers. Every month enrollment is delayed, physician practice groups and health systems lose an average of $100,000 for a single primary care provider. For specialty care, the losses are even more staggering at $300,000 per physician per month.
- Delayed payment or reimbursement: CMS can fine health plans up to $25,000 per Medicare beneficiary for errors in Medicare Advantage plan directories, and up to $100 per beneficiary for mistakes in plans sold on the Affordable Care Act (ACA) exchanges. Health plans, in turn, require health systems to update provider data regularly. For example, CA SB 137 requires health plans to maintain accurate provider directories and update those directories weekly. Health plans reach out to healthcare organizations every six months to validate the accuracy of provider information. A healthcare organization’s failure to respond to these health plan inquiries can result in severe penalties: removal from the provider directory, delay of payment or reimbursement, or even termination of the provider contract.
- Rejected claims and reimbursement delays: Incorrect addresses for outpatient service locations may lead to denied claims, lost revenue, and costly claim resubmissions. Medicare rejects claims when there is not an exact match between the address information submitted on the hospital’s CMS Form 855A (and appearing in PECOS) and the off-campus hospital outpatient departments service facility location reported on the hospital’s Medicare Outpatient Prospective Payment System claims. Even slight discrepancies in the addresses—“Rd” or “Ste” instead of “Road” or “Suite”—will cause claims to be rejected.
Hospitals could lose millions of dollars—that’s up to $16 million for a large integrated delivery network (IDN) with 121 hospitals, assuming a 10% data discrepancy. Or, at the very least, the IDN could wait months to receive money from CMS. This may result in temporary cash flow problems. If the addresses don’t match exactly, hospitals will receive a return-to-provider notice. Billing staff will have to work with their Medicare Administrative Contractor to revise and resubmit the claims. This process is time-consuming and expensive: $118 is the average cost to reprocess a single claim. In the worst-case scenario, billing departments may miss the window to file claims. Under the ACA, claims must be filed within one year from the date of service to be paid.
To prevent these problems, healthcare organizations devote considerable time and resources on provider data management technology to maintain accuracy. The U.S. healthcare industry spends $2.76 billion per year—about $1,000 per month, per practice—to maintain provider directories, according to a survey conducted by the Council for Affordable Quality Healthcare.
Real-time provider data increases efficiency
More staff across hospitals and health systems require access to provider data, for an increasing number of reasons. Unfortunately, in most healthcare organizations, that information is stored in different departments in disparate systems—like contracting, HR, credentialing, quality—that don’t share data. Personnel in the medical staff office waste hours tracking down provider data from multiple sources and repeatedly asking physicians for updated information.
When medical staff offices and other authorized users have access to real-time provider data via provider data management technology, managing that data becomes easier for the many activities it enables. Some of the functions that benefit from the use of an integrated and consolidated provider data management software system include the following:
- Generating and processing initial applications from providers
- Maintaining physician employment contracts
- Enrollment, re-enrollment and un-enrollment with multiple health plans for each provider
- Credentialing and privileging
- Updating provider directories
- Enabling provider self-service for managing their information
- Giving physicians’ leaders the ability to conduct virtual committee meetings
- Peer review, including ongoing/focused professional practice evaluation (OPPE/FPPE)
- Tracking physicians’ continuing medical education
- Tracking physicians’ maintenance of board certification
- Linking privileges to ICD/CPT codes for billing and quality purposes
- Linking provider credentialing, EHR, directory, and claims data
- Enabling real-time provider search for staff (i.e., privilege lookup) and patients (i.e., patient-provider matching)
- Supporting patient access and referral management
How to achieve provider data management efficiencies
There’s a tipping point when manual processes or insufficient provider data management technology becomes detrimental to your healthcare organization. It hampers the ability to grow the business, ensure data security, cut overhead costs, improve workflow accuracy and speed, and enhance provider/patient satisfaction.
Here are the drivers of efficiency you should expect from your provider data management solution.
1. Automation
Provider data management software interacts with CAQH for fast provider profile updates and includes web crawlers that obtain practitioner data through state licensure, the U.S. Drug Enforcement Administration, the Office of Inspector General, National Practitioner Data Bank, and other authorities. Other time-saving tools built into an automated provider lifecycle solution can send applications in batches and verify in batches (multiple facilities, providers, verification types) to accelerate credentialing and enrollment on a large scale.
2. Mobility
Secure, paperless, mobile access is required as the new way to restructure the credentialing, privileging, enrollment, and committee participation functions. Using data stored in the cloud, it’s the best way to avoid disruptions and minimize compliance risks when patients, staff, and clinicians are geographically scattered.
3. Reinforcement
Sometimes interim help is needed to clear a backlog of files, get to paperless, or handle spikes in provider volume due to acquisitions or mergers. With integrated provider data management, your files are automatically saved in a shared database on a web server, allowing authorized reinforcement staff to access the system. It enables users to assign permissions and access levels while still maintaining control and security of provider data.
4. Analytics
When provider data is integrated, the ability to create more precise reports and analytics is enabled for better decision making. Valid data and insights such as the following are gained enterprise wide:
- Providers with expiring items in the near future
- Providers with re-appointments in the upcoming months
- Quality performance details of providers by department or specialty
- Auditing requests for regulatory bodies
5. Customization
Integrated provider data management software carries most of the effort for applications (i.e., provider initial appointment and reappointment, and payer enrollment). The sheer number of application types requires automation and standardization to map applications, run reports, or create custom fields capable of more than just “yes/no” responses.
6. Customer service
Holding on to multiple systems that house provider data or even partially using paper processes negatively affects customer service and marketing for your healthcare organization. Internal and external customers may view your paper processes as outdated and not secure or confidential.
7. Centralization
The use of one source of truth for provider data management eliminates data duplication and repetitive tasks, and allows for easy knowledge transfer among authorized users. Further, centralizing provider data fosters the ability to communicate more effectively in sharing data, ensuring data integrity and transparency, and demonstrating accountability for large volumes of traceable data.
8. Security
Data security requires vigilance over administrative, physical, and technical entry points. Cloud-based provider data management vendors consistently invest in security and are often better equipped than internal IT departments to address unique provider data privacy and security needs. A few examples include encryption, application of administrative permissions, and installation of security features that meet federal, state, and board regulations.
9. Cost effectiveness
By eliminating the use of paper files and storing your provider data safely in the cloud, your organization avoids delays that slow reimbursement timelines, improves the efficiency of staff, and improves the bottom line. Often-overlooked costs associated with paper are offsite data storage, mailing costs, and environmental printer and ink disposal fees.
10. Compliance
Failure to submit required documentation on time draws fines and jeopardizes accreditation and compliance. A fully digital provider data management solution creates alerts, reminders, and automated workflows that ensure no step in the credentialing or enrollment process is missed.
Contact us today to find out what efficiencies you could uncover to achieve accurate, more cost-effective provider data management in your hospital or health system.