Proven Strategies for Health Systems to Contain Premium Labor Costs

As a Customer Success Manager, I’ve seen firsthand how important it is for health systems to find the balance between flexing their staffing plans to meet patient care needs and protecting the bottom line. When patient census and/or acuity increase or staff call in sick, unit leaders need to quickly find qualified staff to fill the gaps. Often, that requires the manager to rely on premium labor to incentivize staff to fill the open shifts at the last minute.
Unfortunately, premium labor expenses are not just a tool to fill last-minute open shifts; instead, in some health systems, schedules are created with a heavy reliance on scheduling staff for overtime.
Whether planned or not, premium labor can have a negative impact on the budget at both the unit and system level. I’ve also seen how premium labor can take a toll on both staff and patients.
Let’s take a closer look at the definition, causes, and cures for premium labor.
Different Types of Premium Labor
Here are four types of premium labor found in many hospitals and health systems:
1. Agency/Traveler
This contract labor can be used to supplement limited internal resources to fill the gaps. While agency and traveler staff are sometimes necessary when your organization doesn’t have enough internal staff to meet patient demand and achieve appropriate staffing levels, it is very expensive labor.
2. Overtime
Whether it’s scheduled or unscheduled, there’s lots of preventable overtime in hospitals. One type of overtime that is often overlooked is incidental overtime, which happens in short 10 to 60-minute increments when an employee arrives a little early or stays a little late. The financial impact of incidental overtime is anything but incidental – we’ve found that it accounts for about 5 to 10% of total overtime expenses. Here’s a blog post that shares strategies for reducing incidental overtime.
3. Incentive Pay
In a study Symplr conducted with Becker’s Healthcare, we found that the number one workforce management initiative to boost staff engagement was using incentive programs to fill open shifts. This can be costly, and it needs to be done very strategically. It can be beneficial to lean on internal staff before booking agency, but the strategy needs to be reviewed constantly or over time, bad habits can be established and become the norm. I’ve seen hospitals that use incentives strategically to save thousands or even millions of dollars in contract labor reductions, but I have also unfortunately seen the incentive programs slip out of control and become a high, unexpected cost. For example, you don’t want staff holding out to the last minute because a large bonus on a shift is expected. Instead, you want to offer the bonuses up front, early on, to minimize the last-minute chaos.
4. Missed Meals
When employees miss their lunch, it often leads to overtime. In some instances, focusing on minimizing the number of missed lunches can be a quick way to cut premium labor costs without having a negative impact on patient care.
The Negative Impacts of Premium Labor
It’s clear that premium labor has a negative impact on the bottom line. But, excessive overtime and other types of premium labor can lead to staff dissatisfaction and burnout (check out this blog post for a closer look at nurse burnout). Ultimately, the negative effect on staff impacts the quality of care and patient safety.
Here are some research findings that illustrate the negative impact of premium labor, especially overtime:
- The prevalence of overtime is increasing. The U.S. Bureau of Labor Statistics show that average weekly hours worked in hospitals has reached record highs.
- Labor makes up a bigger percentage of hospital expenses than it did 10 years ago, which worsens the hospital’s financial standing.
- Nurses who work long shifts (12+ hours) are more likely to intend to leave the job than nurses who work shorter shifts.
- When nurses work shifts longer than 13 hours, patients are less likely to recommend the hospital to friends and family. And, they give the hospital lower overall HCAHPS ratings.
Understanding Why Premium Labor is Happening
In order to manage premium labor, it’s important to understand why it’s happening. In addition to some of the reasons outlined above, here are some common systemic reasons that hospitals/health systems find themselves using premium labor:
- Lack of data and visibility – Without the right tools to capture and manage key analytics, it is challenging to find and eliminate the root cause of the premium labor.
- Policy shortcomings – Your staffing and scheduling policies should clearly define the parameters around the use of premium labor, as well as who is accountable for managing it. If there are no clear expectations and accountability in place, staffing leaders can default to filling staffing holes with the most convenient choice rather than the most cost-effective choice, leading to the unnecessary use of premium labor.
- Resource constraints - When an organization is short-staffed, it can be nearly impossible to effectively manage premium labor costs.
- Competition and market conditions – In order to recruit and retain staff, your health system needs to offer competitive wages, which includes incentive plans.
Proven Methodology to Manage Premium Labor Costs
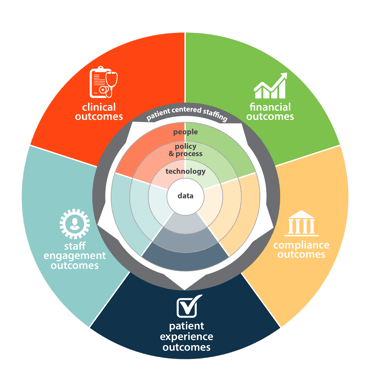
Based on our team’s expertise, input from customers, and recent industry research, we’ve developed a methodology that empowers successful workforce management initiatives, including better management of premium labor costs.
Use Analytics and Take Advantage of Technology Tools
The process starts with leveraging technology and using data to find the issues and determine the root causes. You need to understand where there is overtime and premium labor spend and why it’s happening. Is it resource constraints? An uptick in census?
Using analytics is a really good way of taking both a high-level view and a deep dive into workforce performance, premium labor spending and monitoring. In the ever-changing, competitive, thin-margin healthcare realm today, it creates a huge advantage to be able to visualize the data about how your workforce is being planned and managed.
Here are a few areas to examine in the search for the sources of premium labor:
- Staff utilization
- Incidental overtime
- Badging and timecard approval compliance (data latency)
- Not flexing staff based on need, which can be caused by not using census and/or acuity data
- Units that are trouble spots
- Understaffing
- Overstaffing
Success requires more than data. Utilizing the technology available can help reduce unnecessary premium labor costs. Make sure your organization is taking full advantage of tools that give staffers a whole house view of staffing and provide data that enable better decision-making. For example, who is about the best option to call in when there is an open shift? If one unit has low census, should an employee from that unit float to another unit instead of being sent home? Technology tools should make it easy for staffing coordinators and unit managers to make the best choices based on data.
Make the Right Policies a Priority
Your health system should have policies in place so that anyone who is making a staffing decision is following the organization’s defined leading practices. Here are some areas your premium labor polices need to address:
Overtime
- How are staff chosen for overtime? Have staffers tried per diem and part-time staff first?
- Is productivity monitored real-time?
- Is the staffing equitable?
- Is staffing based on the patient need and workload necessary to care for the patient?
Agency/Traveler
- How are these staff contracted?
- Have staffers exhausted all options before resorting to an agency resource?
- Are there specific policies and procedures that need to be followed before using these resources?
These are the types of policies that need to be in place to ensure system wide accountability and knowledge when it comes to premium pay. Here’s an example what can happen when policy and accountability are not aligned. An organization had a policy in place for staff to get paid double-time if they were called in for a shift within 24 hours of the shift, even if they weren’t over 40 hours. This policy soon became a hindrance for filling shifts in advance because employees would wait for the 24-hour window before the shift before agreeing to pick up the shift.
For example, if on Monday a staffer asked someone if they can work Friday, the answer would be, “I don’t know, call me on Thursday.” The end result was that nobody would sign up early for open shifts, which caused a lot of last-minute work, chaos, and stress for staffers. And, it was causing premium labor expenses that could have been avoided. So, it’s important that the policy in place is the right policy.
Putting Policies in Place is a Team Effort
Workforce management impacts every single employee; and it’s important that everyone from the executive team to the front-line staff are engaged and committed to be a part of the solution. This is especially true when you’re building or modifying policies that impact premium labor. You need buy-in from everyone, or things won’t work.
If you don’t already have a shared governance structure in place, now is a good time to take the time to create that essential team. I have seen organizations find great success when they build a workforce governance council that focuses on creating a culture of accountability where expectations are clearly defined. The council also focuses on leveraging the reporting and technology so everyone has the tools they need to meet those expectations. This group should meet monthly at a minimum and should have executive, manager, and staff representation from payroll, finance, clinical, operations, and HR. This kind of shared governance is a great way to set your organization up for success, and not just success, but sustainable success. And, it’s the perfect venue for evaluating, modifying, building, and implementing effective premium labor policies that contain costs, engage and satisfy staff, and lead to a better patient experience.
Success Story: Achieving Balance During the COVID-19 Crisis
Premium labor is a top-of-mind issue for many of our customers right now. Many of them are facing high demand in critical care areas related to COVID-19. Conversely, in other parts of the country, or even in another part of the same health system, census is low, and elective surgeries aren’t being performed. To resolve this imbalance, one of our customers leveraged their historical cross-training infrastructure to upskill ambulatory nurses and staff so they would be prepared to work with expert critical care nurses to meet patient care needs during the projected COVID-19 surge. With this strategy, they were able to avoid furloughs as well as minimize their premium labor spend as much as possible in the challenging circumstances – and, their organization is better prepared for future crises.
Success Story: Leveraging Internal Staff While Minimizing Incentive Pay
Earlier, I mentioned that we did a survey where respondents said that incentive pay was a top employee satisfier at their organization. However, we’ve seen some of our customers successfully use a more cost-effective strategy that offers flexibility instead of incentive pay to encourage staff to fill open shifts. It’s called self-directed floating, which means staff can view and choose to work any available shifts that they are qualified to work, including shifts outside of their home unit. By providing this level of transparency, a not-for-profit community hospital in Tennessee has seen voluntary floating become an integral part of filling open shifts, with employees who voluntarily work in a non-home department filling almost 30% of in-patient nursing shifts. In addition, regular internal staff fills shifts at 26% beyond the minimum scheduling requirement, which has greatly reduced the organization’s agency use and costs.
Having an Impact at Your Health System
Managing premium labor expenses requires a strong strategy and the right tools, policies, processes, and people to support that strategy. With the bottom line, staff engagement, and patient satisfaction on the line, managing premium labor has long been a top priority for health systems. Within the context of COVID-19, there’s a growing sense of urgency for health systems to optimize their staff so premium labor expenses are minimized while staff and patient satisfaction are protected.
Are you interested in working with our optimization experts to explore how your health system use data, technology, policies, processes, and people to manage your premium labor costs better? Request a complimentary assessment today, and our team will help you develop a targeted plan for your organization.